Introduction
Multimodality treatment for liver tumours is currently available owing to developments in hepatectomy and other therapies [1, 2]. However, the clinical course often requires multiple surgeries. The value of repeat hepatectomy after liver tumour recurrence following initial hepatectomy has been widely reported in recent years. An increasing number of studies also report the value of laparoscopic rather than open repeat hepatectomy (ORH) [3, 4].
Laparoscopic surgery has been shown to provide good therapeutic outcomes compared with open hepatectomy, mainly because of its lower invasiveness and better cosmetic outcomes [5]. This procedure has undergone dramatic development as a result of advances in instrument design and improved surgical techniques, and it is currently considered an alternative to conventional open surgery. One such surgical technique is the Pringle manoeuvre, which occludes the inflow of blood into the liver. Inflow occlusion is extremely effective in reducing the amount of intraoperative haemorrhage during liver transection [6, 7]. However, in laparoscopic repeat hepatectomy (LRH), outcomes of previous surgery and the influence of other factors frequently make it difficult to occlude the inflow of blood.
Surgical devices have undergone rapid development in recent years, and laparoscopic techniques are improving and becoming standardized [8]. However, the role of blood inflow occlusion in LRH remains unclear, and evidence is still lacking.
Aim
Thus, in this study, we aimed to discuss the value of inflow occlusion during LRH and provide tips for its performance.
Material and methods
Patient population and selection
Between February 2012 and December 2019, 63 consecutive patients who underwent LRH for liver tumours at Osaka Medical College Hospital, were enrolled in this study. All 63 patients underwent laparoscopic repeat liver resection without any other concomitant surgical procedures (i.e. colorectal resection). All patients were fully informed of the study design, which was approved by the Ethics Committee on Clinical Investigation of Osaka Medical College Hospital (approval numbers 1828 and 1997), and they each provided written informed consent. The Pringle manoeuvre was not performed in a total of 19 cases, and 44 patients for whom taping was judged impossible due to adhesions in the hepatic portal area.
A tumour size less than 10 cm was the main criterion when considering a patient for LRH, and the number of tumours and their location were not considered. The indication for LRH was no more than 5 hepatic resection sites. Patients with tumour invasion into adjacent organs were not considered candidates for LRH. Moreover, LRH was not considered for candidates when any complications occurred after the initial hepatectomy. The criteria for conversion from LRH to ORH were as follows: (1) the stumps of both the preserved and resected livers could not be adequately expanded, (2) uncontrollable intraoperative bleeding, (3) blood loss > 500 ml, (4) total Pringle manoeuvre (hepatic blood flow occlusion) time > 120 min, (5) and intraoperative bile leakage not amenable to laparoscopic repair. Patients who required conversion from LRH to ORH were analysed as part of the LRH group.
Surgical procedure
The detailed laparoscopic technique routinely used in our department has been described in previous reports [1, 2, 4, 5]. With abdominal ultrasonography, we assessed the tumour for the presence of abdominal wall adhesions, after which the first trocar was placed at a site that was deemed to be free of adhesions. After the introduction of a 12-mm umbilical or other port using an open technique, continuous carbon dioxide (CO2) pneumoperitoneum was induced at a pressure limit of 12 mm Hg and flow of 6 l/min to decrease the risk of gas embolism. Four 5–12 mm trocars and a 30° laparoscope (1588 AIM; Stryker Japan K.K., Tokyo, Japan) were inserted. Port positioning was standardized according to the hepatic segments to be resected. After identifying any adhesions of the hepatic vein root, diaphragm, or hepatic portal region, a routine diagnostic and staging laparoscopy was performed. Mobilization of the liver was subsequently initiated. The lateral hepatic attachment and the triangular ligament were divided using the surgical tissue management system (Thunderbeat; Olympus Inc., Tokyo, Japan) after the round and falciform ligaments were dissected. This dissection was typically carried up to the diaphragm, allowing more effective mobilization of the liver. In mobilizing the liver, we preserved the liver membrane as much as possible, i.e. even if some of the anatomy was lost due to adhesions, the liver membrane could be preserved, and other organs such as the intestinal tract and diaphragm would not be damaged. Moreover, we performed an extracorporeal Pringle manoeuvre, by occluding the blood flow with a vascular occlusion tube (Vessel-Clude; Argon Medical Devices Inc., USA) from outside the body after any adhesions of the hepatic hilar region were identified (Figure 1). In addition to intraoperative ultrasonography, laparoscopic ICG-fluorescence imaging was also used to determine the demarcation line and to identify the tumour. The central venous pressure was maintained at 0–3 mm Hg during parenchymal transection. Parenchymal transection was performed using the Sonop 5000 ultrasonic dissector (Hitachi Aloka Medical, Ltd.) and the surgical tissue-management system. The stumps of the liver transection line on both the preserved and resected sides were adequately expanded. Small vessels were ligated or coagulated using a soft-coagulation system. Intraparenchymal control of major vessels was obtained with non-absorbable sutures, whereas biliary and vascular radical division was accomplished with stapling devices or non-absorbable sutures. The hepatic pedicle was always isolated to enable use of the Pringle manoeuvre if possible. Intermittent clamping was applied with 15-min clamping and 5-min release periods. During the resection, the surgical margin was carefully confirmed using intraoperative ultrasonography to obtain a margin of 5–10 mm when possible. The resected, undivided specimen was placed in a plastic retrieval bag and removed through the umbilical incision.
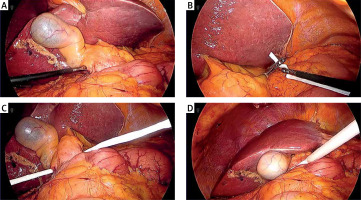
Figure 1
Placement of extracorporeal Pringle manoeuvre during laparoscopic hepatic resection. A – The round ligament of the liver is elevated, and the hepatoduodenal ligament is opened. For confirmation, a thorough inspection is performed for the presence of adhesions around Winslow’s foramen. B – The inferior vena cava location is confirmed. The forceps is inserted between the inferior vena cava and the hepatoduodenal ligament. The forceps is inserted toward the direction of the lesser omentum. The edge of the cotton tape is grasped with the forceps once the latter has been pulled out from the lesser omentum. C – The cotton tape is pulled out and passed behind the hepatoduodenal ligament. D – The edge of the cotton tape is pulled out from the port wound in the left upper abdomen. The cotton tape is inserted into the abdominal cavity by passing it through a Vessel-Clude*. The preparations for the extracorporeal Pringle manoeuvre are complete
Definitions
The “R” classification denoted the absence or presence of a residual tumour postoperatively [9]. Morbidity was graded according to the Clavien-Dindo classification. Surgical site infections were defined according to the Centre for Disease Control’s National Nosocomial Infection Surveillance system [10]. Postoperative bile leakage and post-hepatectomy liver failure were defined according to the criteria of the International Study Group of Liver Surgery [11, 12]. We defined massive ascites as ascites that could not be managed or satisfactorily prevented with medical therapy [13]. The extent of hepatic fibrosis was scored as follows: stage 0, no fibrosis; stage 1, portal fibrosis without septa; stage 2, portal fibrosis with rare septa; stage 3, numerous septa without cirrhosis; and stage 4, cirrhosis [14].
Statistical analysis
To minimize the influence of potential confounders on selection bias, propensity scores were generated using binary logistic regression, which included the following variables: age, sex, body mass index (BMI), pathological diagnosis, viral hepatitis infection status, presence of diabetes mellitus, total bilirubin, albumin, prothrombin time (PT), platelet count, indocyanine green retention rate at 15 min (ICG-R15), Child-Pugh classification, tumour number, largest tumour size, tumour location, and number of hepatic resections. One-to-one matching between the groups was accomplished using the nearest-neighbour matching method, which was performed without replacement and using a calliper width of 0.2 standard deviations of the logit of the estimated propensity score. After propensity score matching (PSM), the 2 matched groups were handled as unpaired independent groups. Continuous variables are expressed as medians ± standard deviation. Continuous variables were compared using Student’s t-test and Mann-Whitney U test. Univariate analyses of categorical variables were performed using the likelihood-ratio test or Fisher’s exact test, as appropriate. Factors that were found to be significant in the univariate analysis were subjected to a multivariate logistic regression analysis to determine the adjusted odds ratios. P < 0.05 values were considered significant. All statistical analyses were performed using JMP version 14 (SAS Institute, Inc., Cary, NC, USA).
Results
Patient demographics
In all 63 patients, the procedure was successfully completed laparoscopically in 57 patients. However, 6 (9.5%) patients underwent conversion to open surgeries. This was due to bleeding in 3 patients and intra-abdominal adhesions in 3 patients. In most of the patients in the LRH group with the Pringle manoeuvre, the number of tumours and amount of excised liver was large, and the conversion rates to ORH were high. Therefore, to avoid selection bias between the 2 groups, a comparative study was carried out by using one-to-one PSM. According to PSM, 15 of the 19 patients in the LRH group with the Pringle manoeuvre were matched with 15 of the 44 patients in the LRH group without the Pringle manoeuvre. The baseline characteristics of the matched study population (30 patients) are summarized in Table I. No significant differences in the demographic or operative characteristics were found between the groups. After PSM, in the LRH group without Pringle manoeuvre, the laparoscopic procedure was successfully completed in 12 patients. However, 3 (20.0%) patients required conversion to ORH because of bleeding from a hepatic vein branch and adhesions that could not be removed laparoscopically (p = 0.034). However, no significant difference was found between the 2 groups in terms of the duration of surgery, estimated blood loss, and postoperative complication rate (Clavien-Dindo grade > IIIA) (p = 0.973, p = 0.120, and not applicable, respectively).
Table I
The baseline characteristics and surgical outcomes of the study population who underwent laparoscopic repeat hepatectomy
[i] Data was presented as median (range), *P < 0.05, apercentage (%) of the group, PSM – propensity score matching, BMI – body mass index, VFA – visceral fat area, SFA – subcutaneous fat area, HCC – hepatocellular carcinoma, ICGR-15 – Indocyanine green retention rate at 15 min, PNI – prognostic nutritional index, CD – Clavien-Dindo, PHLF – post-hepatectomy liver failure, NA – not applicable.
Postoperative aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels peaked on day 1 and had almost normalized on day 7. Postoperative serum albumin, white blood cell (WBC) counts, C-reactive protein (CRP) levels, PTs, and platelet counts peaked on day 2 and then gradually normalized. Postoperatively, total bilirubin, serum albumin, PTs, platelet counts, AST, ALT, WBC counts, and CRP levels, especially on the peak day, were significantly lower in the LRH group than in the ORH group (p = 0.479, p = 0.670, p = 0.499, p = 0.403, p = 0.481, p = 0.705, p = 0.608, and p = 0.485, respectively).
Risk factors for conversion from LRH to ORH
Perioperative factors were compared between patients with and without conversion to ORH. No significant correlation was found between the initial hepatectomy carried out as open surgery or laparoscopically and conversion to ORH from LRH (p = 0.326). Moreover, no association was noted between the initial resection involving the right or left lobe and conversion to open hepatectomy (p = 0.250), nor was there any association with the initial and repeat hepatectomies involving lobes on the same side or on opposite sides (p = 0.738). The two significant correlations observed in the univariate analysis were between the history of cholecystectomy, use or non-use of the Pringle manoeuvre, and conversion to open hepatectomy (p = 0.039 and 0.032), although no significant correlation was found in the multivariate analysis.
Of the 44 patients in whom the Pringle manoeuvre could not be performed, 28 (63.6%) had undergone cholecystectomy (p < 0.001) and 18 (40.9%) had undergone segment 5 resection of the liver (p = 0.017). However, no association was observed between the use of the Pringle manoeuvre and whether the initial hepatectomy had involved the lobe on the same side or the opposite side to that involved in the repeat hepatectomy (p = 0.154). In addition, no association was found between the initial hepatectomy carried out laparoscopically or as open surgery and the use of the Pringle manoeuvre (p = 0.094) (Table II).
Table II
Risk factors for conversion from laparoscopic to open repeat hepatectomy
Discussion
In this study, the rate of conversion to open surgery was significantly lower in the Pringle manoeuvre group. In particular, in many cases the cause of conversion from LRH to ORH was the non-use of inflow occlusion and the resulting inability to control intraoperative haemorrhage. This suggested that inflow occlusion is important in laparoscopic repeat haemorrhage.
The Pringle manoeuvre is currently used in most hospitals to counteract intraoperative haemorrhage in laparoscopic hepatectomy by occluding the flow of blood to the liver. The Pringle manoeuvre was first reported by Pringle in 1908 as a method of hepatic inflow occlusion in open surgery and is now widely used worldwide [15]. In repeat hepatectomy, however, adhesions, stemming from operations during the initial hepatic transection or cholecystectomy, mean that anatomical landmarks in the portal region are lost, increasing the risk of damage to blood vessels, bile duct, stomach, duodenum, intestinal tract, and other organs during hepatic inflow occlusion [16]. Many hospitals thus perform liver transection without the use of the Pringle manoeuvre to occlude the inflow of blood during LRH.
In our hospital, we take various measures to enable inflow occlusion safely. First, whenever possible, we spare the gall bladder in initial hepatectomy. When the gallbladder is removed, the gap between the hepatoduodenal ligament and the inferior vena cava on the right side of the hepatoduodenal ligament often adheres, and the stomach, duodenum and transverse colon often adheres to the liver bed. Therefore, by preserving the gall bladder as much as possible and spraying an anti-adhesion agent around the entire circumference of the hepatoduodenal ligament, we reduce the severity of adhesions in the portal region during subsequent hepatectomy, making it more likely that inflow occlusion can be performed in the future.
If the previous hepatectomy has involved the transection of the left lobar system, adhesions tend to occur between the cut surface of the liver and the stomach and duodenum. However, if it involved the right lobar system, the duodenum, colon, retroperitoneum, and omentum tend to adhere to the portal region. By preserving as much as possible the hepatic capsule and gastrointestinal serosa, while detaching the portal region, we ensure that a few of the landmarks lost to adhesions can be identified, and we carefully avoid damaging other organs.
However, regardless of whether the initial hepatectomy was open or laparoscopic, adhesions in the portal region may interfere with the taping of the hepatoduodenal ligament required to perform the Pringle manoeuvre. In this case, we use a detachable Endo intestinal clip to compress the hepatoduodenal ligament and occlude the hepatic inflow. In this process, we open up the left side of the portal region (lesser omentum) in an effort to identify the hepatoduodenal ligament. Even if adhesions from previous surgical operations are present, in most cases, inflow occlusion can be performed via an approach from the opposite side to the previous hepatectomy.
If inflow occlusion is not feasible, we take measures to deal with venous haemorrhage by increasing the pneumoperitoneum pressure, reducing central venous pressure, decreasing tidal volume, and decreasing positive end-expiratory pressure [17–19]. Although our basic policy is to occlude hepatic inflow when transecting the hepatic parenchyma, we have found that even if this is infeasible, the use of other measures to prevent bleeding enable us to reduce intraoperative haemorrhage and perform the surgery safely while keeping the transection stump of the liver dry. However, this study has some limitations. This study did not examine a large number of cases and thus may have been biased in terms of the characteristics of the liver tumours, type and quality of the hepatectomies, and other factors. In addition to accumulating more cases, randomized controlled trials and meta-analyses should be performed in the future.
Conclusions
These tips for various surgical procedures enable safer performance of hepatic inflow occlusion during LRH. Although we found no difference in operating time, estimated blood loss, or incidence of postoperative complications compared with patients in whom the Pringle manoeuvre could not be performed, the rate of conversion to open surgery was significantly lower. However, it is often challenging to perform the Pringle manoeuvre in patients with a history of cholecystectomy, and caution is required.










